Biogen Announcement Highlights Where the Industry is Going Wrong
Dr. Omar El-Agnaf, Executive Director of Qatar Biomedical Research Institute at Hamad Bin Khalifa University, explains why the pharmaceutical industry needs to change its strategy to find an effective drug to tackle Alzheimer’s disease

In the past 20 years, there have been more than 100 attempts to develop an effective drug to treat Alzheimer’s disease, but only four have been approved by the US Federal Drug Authority (FDA) for instance.
In fact, there are currently only two classes of drugs available, and both aim to treat certain symptoms of Alzheimer’s, rather than finding a cure for the disease.
Alzheimer’s is a major worldwide problem. It is a degenerative brain disease and the most common cause of dementia.
The most typical early symptom of Alzheimer’s is difficulty remembering recent events. As the disease advances, symptoms can include problems with language, disorientation (including easily getting lost), mood swings, loss of motivation, not managing self-care, and behavioral issues.
Alzheimer’s is ultimately fatal, with people in the final stages of the disease being bed-bound and requiring around-the-clock care.
Worryingly, the success rate of clinical trials for Alzheimer’s is extremely low, and not enough is being learned from these failures.
This was perfectly demonstrated recently when American multinational biotechnology company Biogen announced that they were halting their clinical trials of a drug that targets amyloid plaques, which are clumps of beta-amyloids that destroy connections between nerve cells.
People with Alzheimer’s have large amounts of amyloid plaques in their brains, so it is essential that research and clinical trials are conducted to enable us to target them.
Biogen, and its Japanese partner Eisai, said they were halting two late-stage clinical trials of the experimental drug Aducanumab after concluding that it was unlikely to benefit patients.
This announcement represents further devastating news for patients with Alzheimer’s disease and their families. It confirmed yet again the complexity of the disease and the need for increased knowledge of the disease biology.
In my opinion, the mistake Biogen made from the start is that they seemed to turn a blind eye to previous failed clinical trials.
The industry needs to pay more attention to previous trials if we are to move forward. For instance, what if some of the failed drugs worked in a subset of patients at the right time? It is time to learn from oncology about how best to conduct trials, and the drug industry should give greater consideration to early detection for early intervention.
It is widely known that beta amyloid - peptides of 36–43 amino acids that are the main component of amyloid plaques - begin to accumulate two decades or so before any sign of clinical symptoms, by which time it is too late to stop the disease’s progression.
We also know that many Alzheimer’s patients at an advanced stage develop not only amyloid plaques and neurofibrillary tangles - aggregates of hyperphosphorylated tau protein - but also other pathologies that are associated with other neurodegenerative diseases and therefore make the treatment of such patients more complicated.
These other pathologies include Lewy bodies associated with dementia with Lewy bodies - a type of dementia that is accompanied by changes in behavior, cognition, and movement; and TDP-43, which plays a pathogenic role in both amyotrophic lateral sclerosis and frontotemporal dementia. Therefore distinguishing between different types of neurodegenerative conditions is important as it enables us to determine the best approach to treatment.
If there is a positive to come from this latest devastating news for Alzheimer’s patients and their families, it is that it may force the pharmaceutical industry to focus on other strategies. It is time to step away from the ‘one size fits all magic bullet’ approach of developing Alzheimer’s drugs, and instead adopt Alzheimer’s precision medicine.
Precision medicine has led to breakthroughs in the treatment of cancer, but it can also help foster innovative thinking to tackle a wide range of complex diseases, including Alzheimer's.
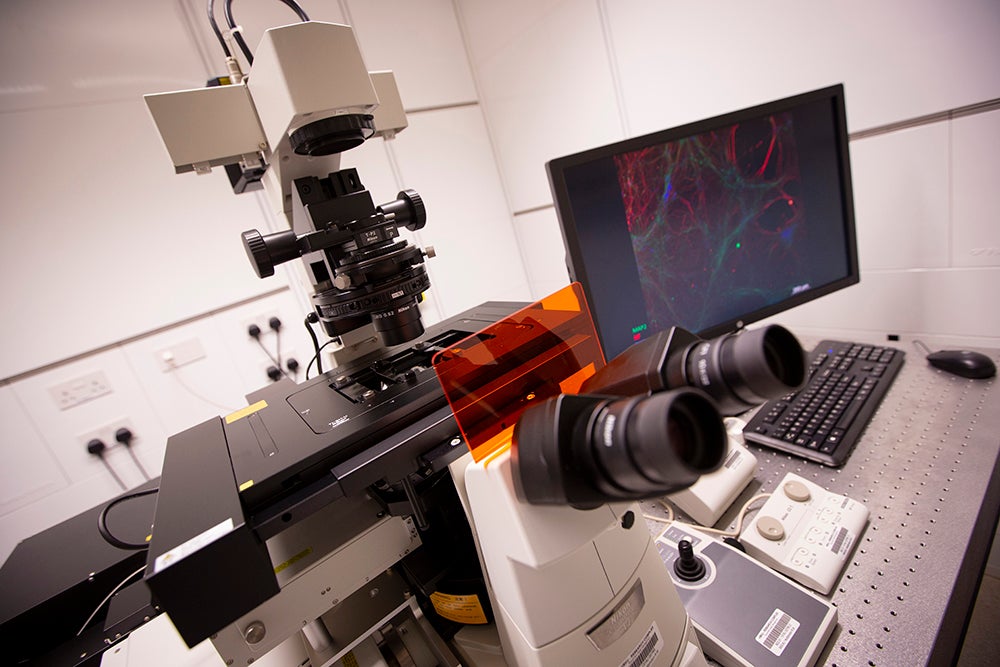
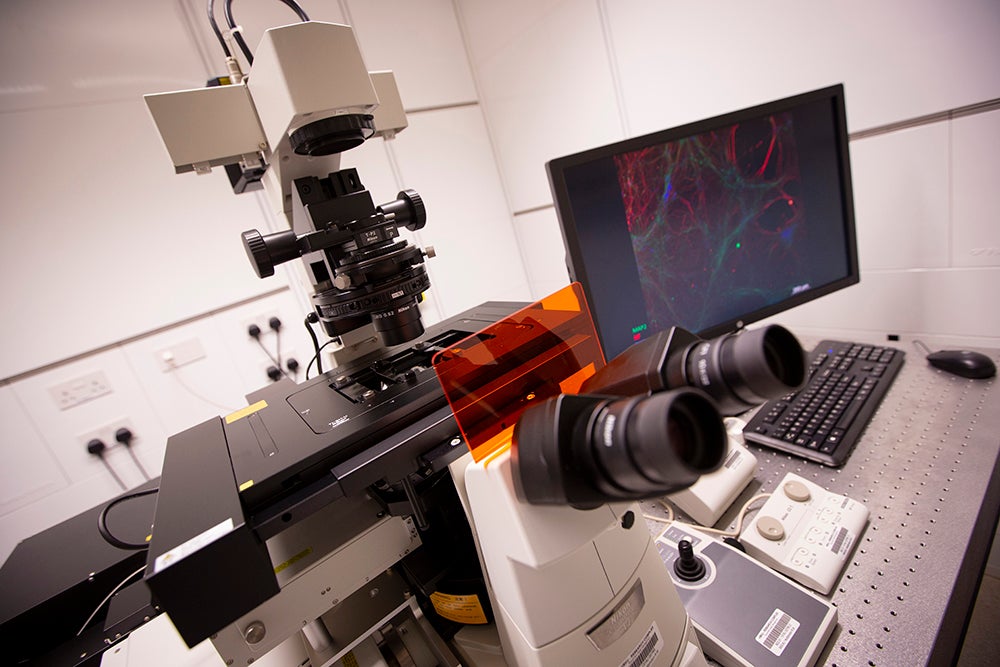
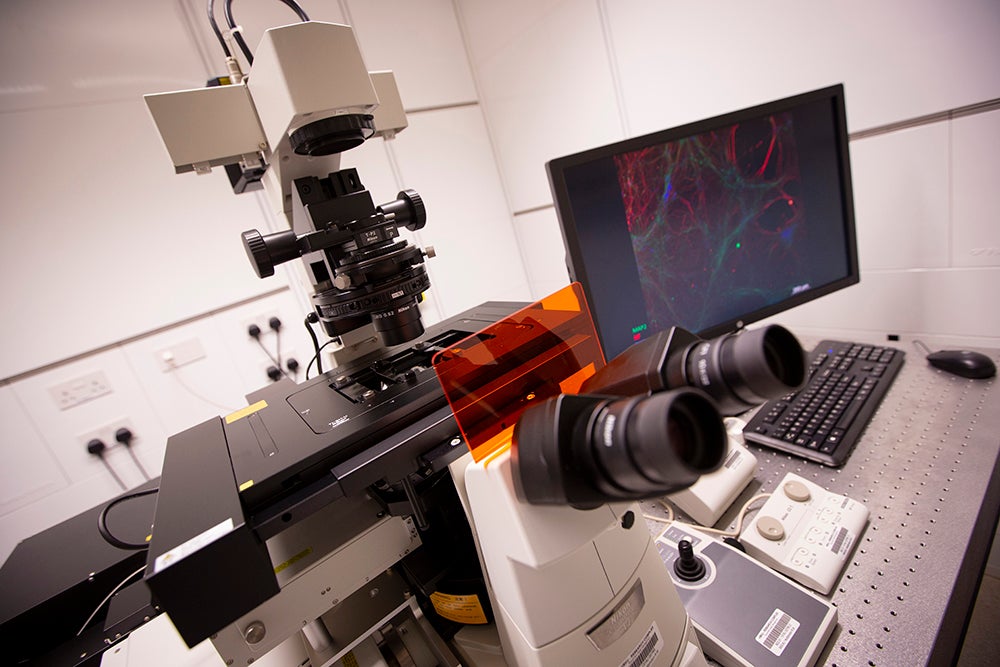
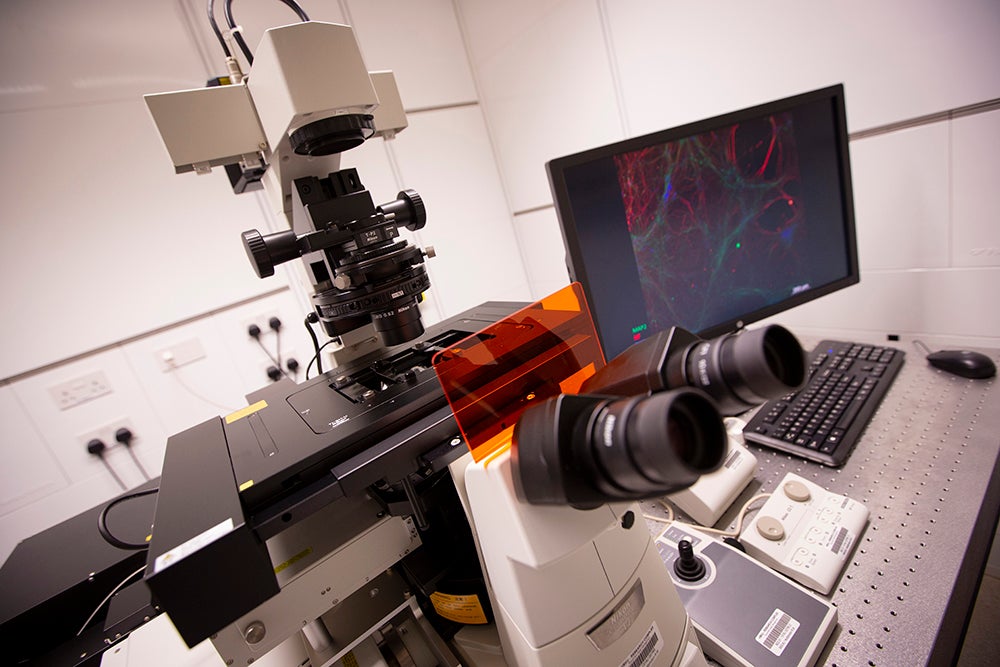
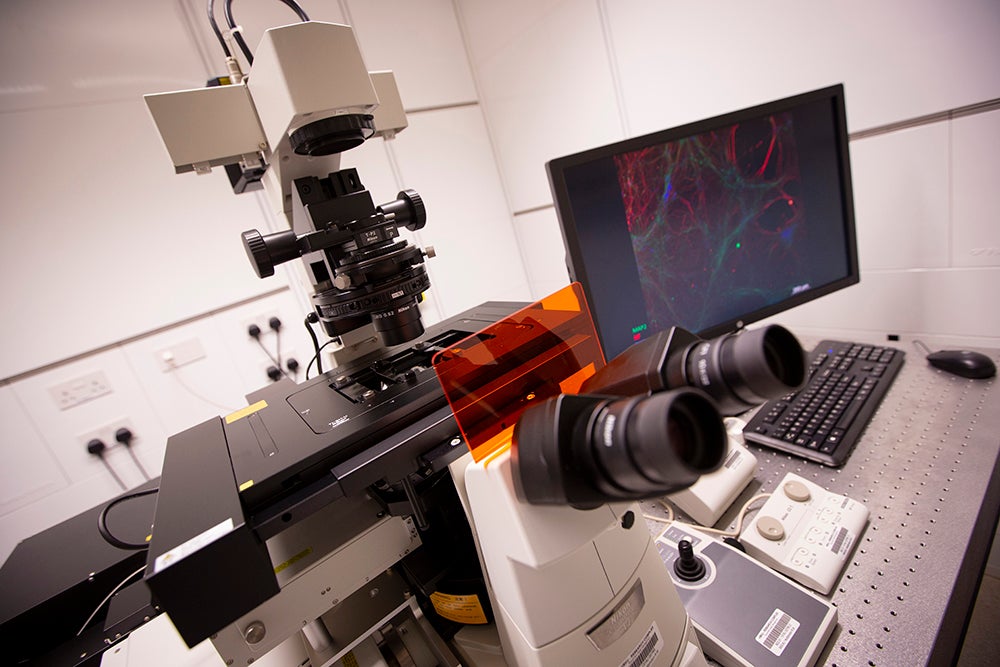
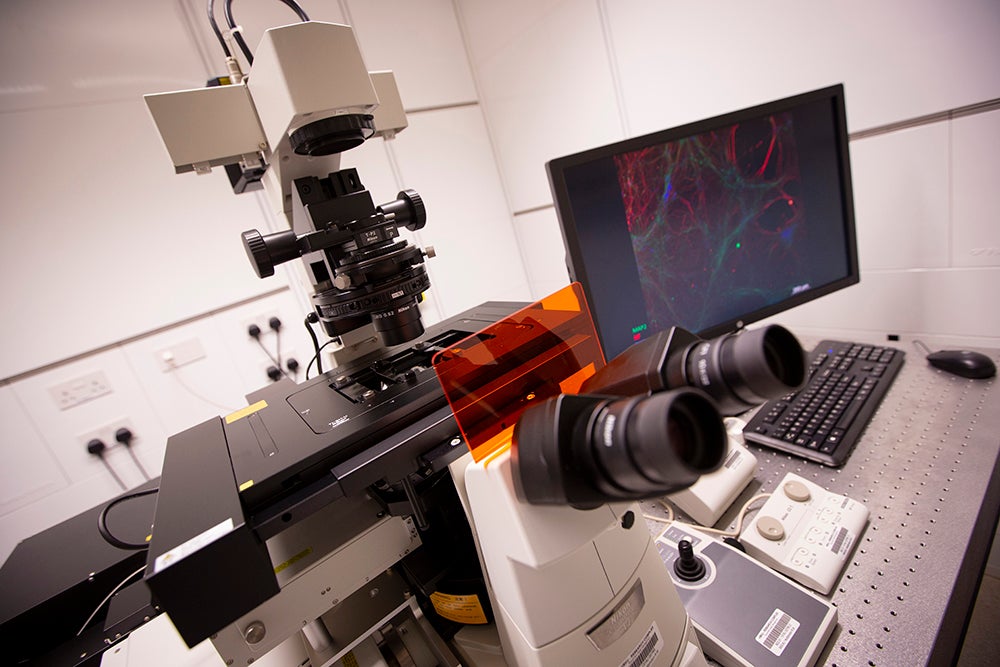
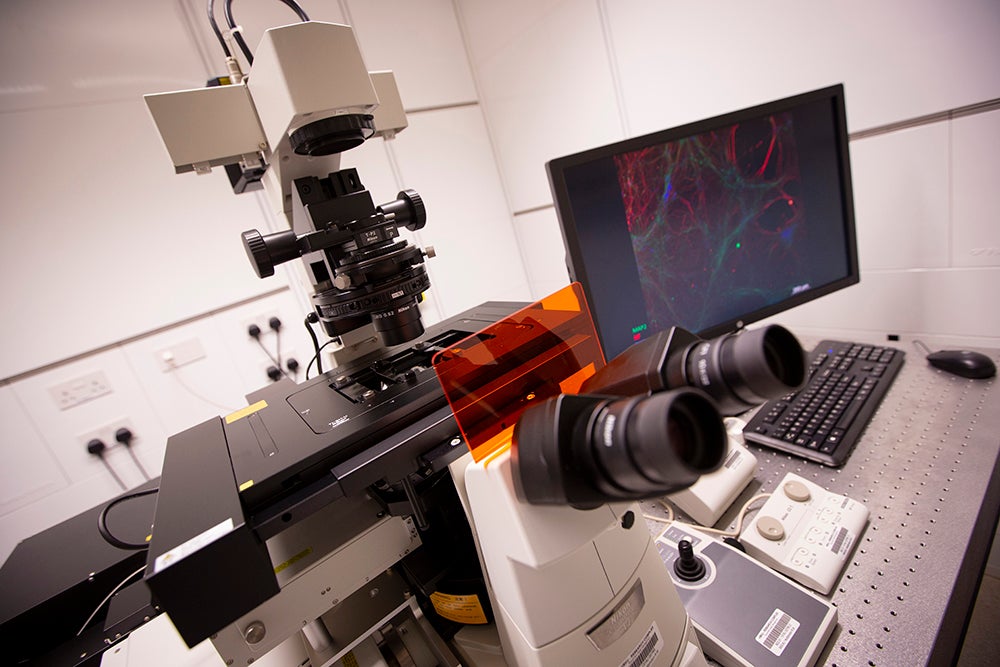
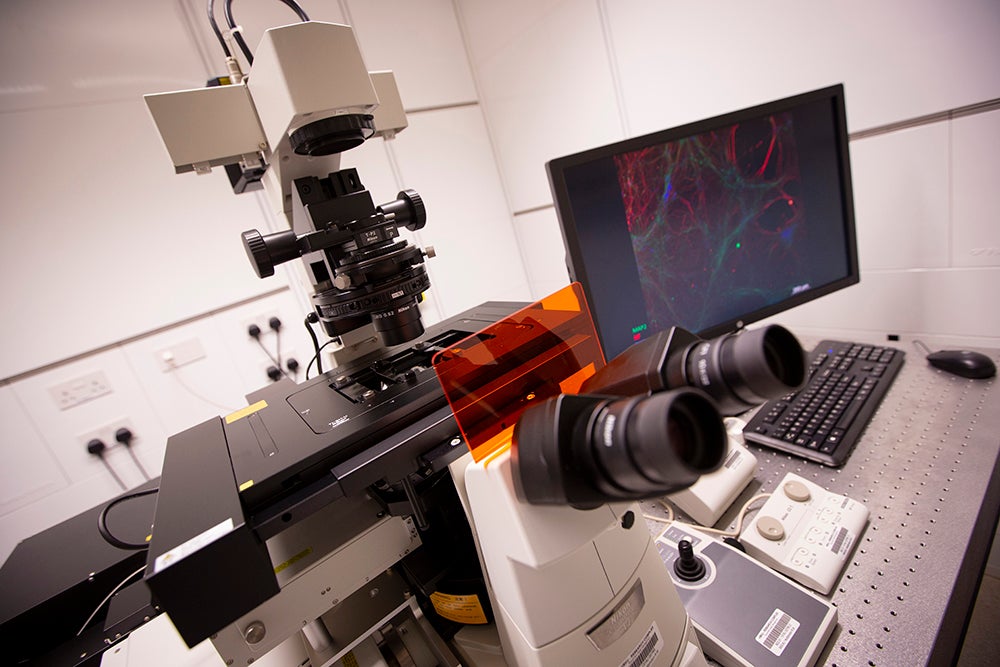
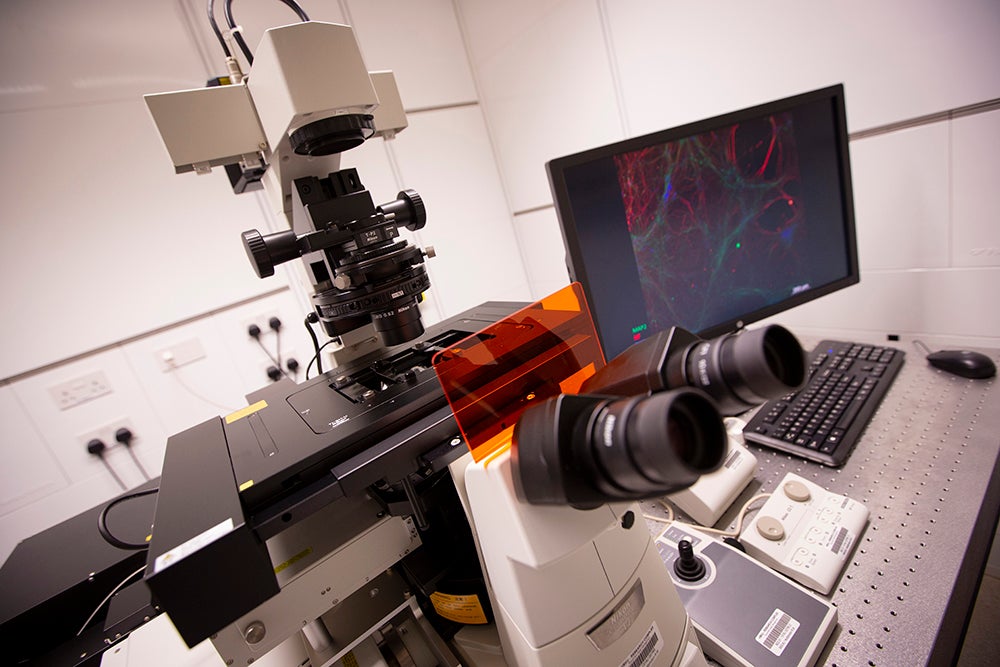
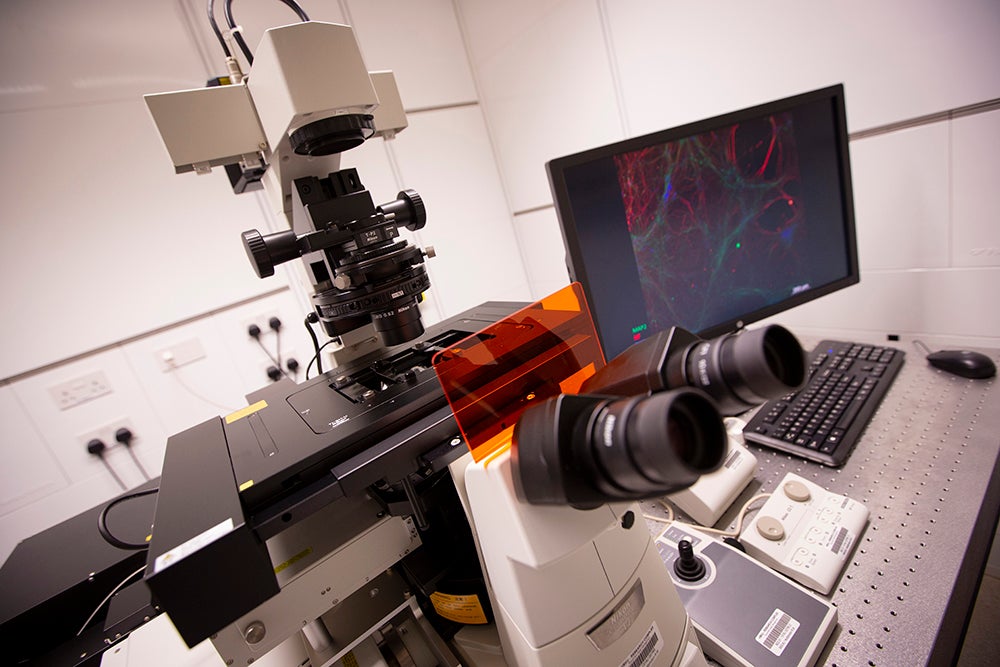
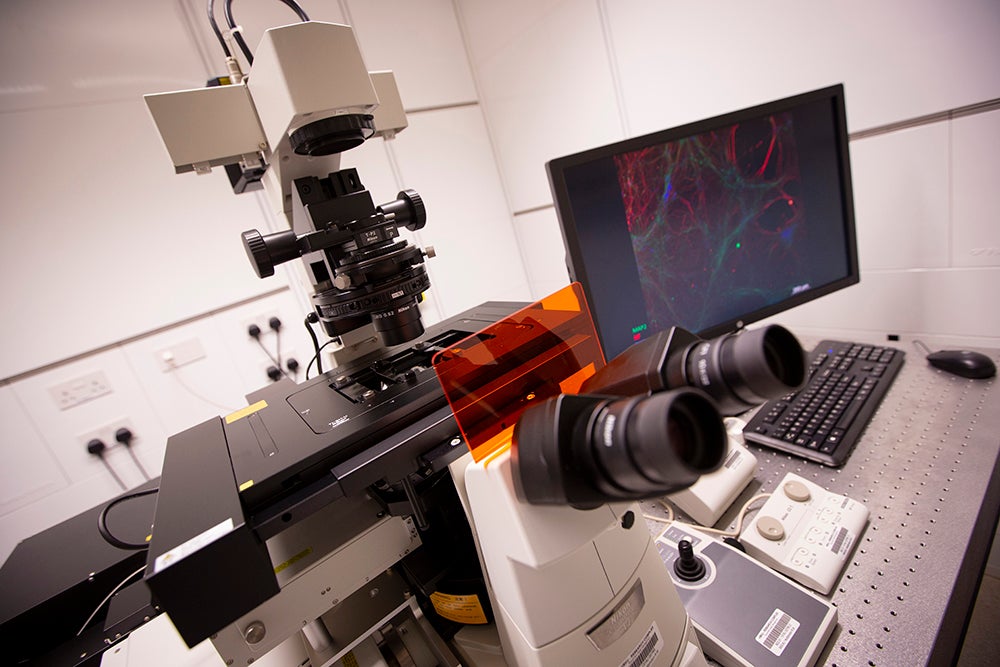
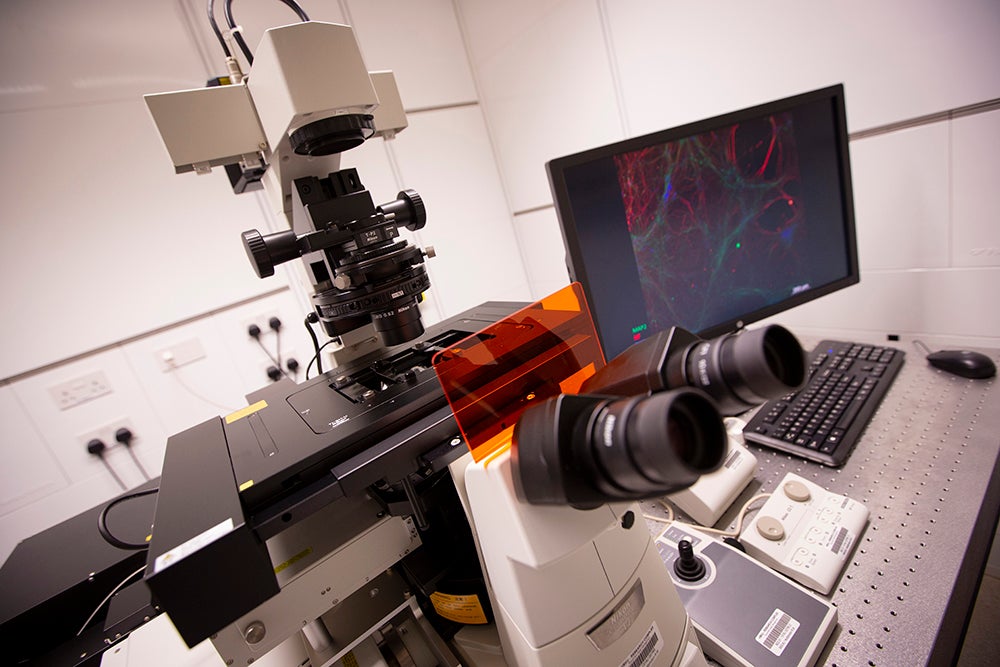
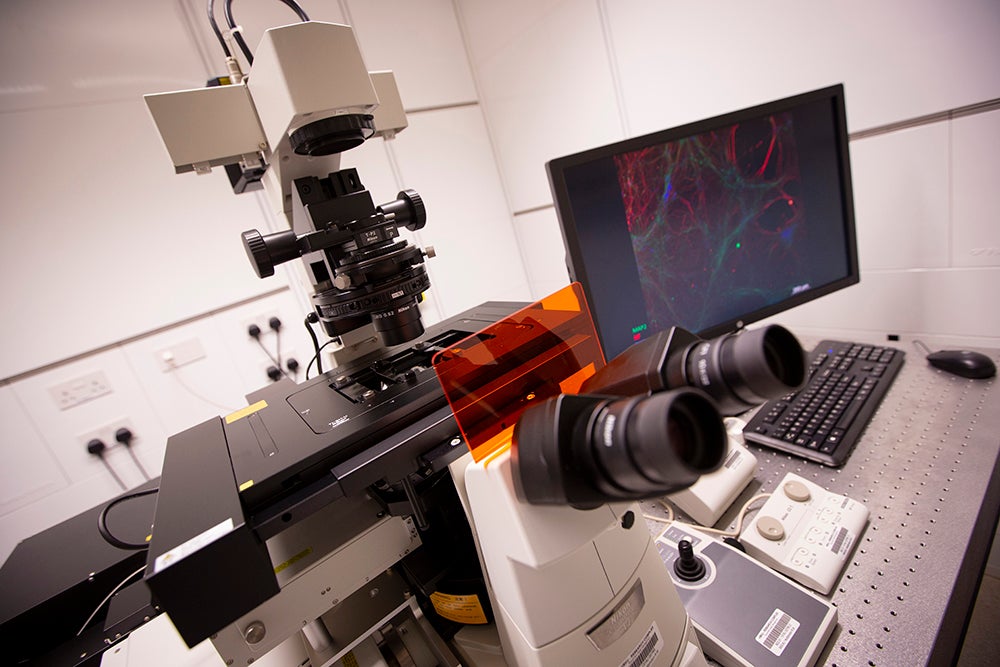
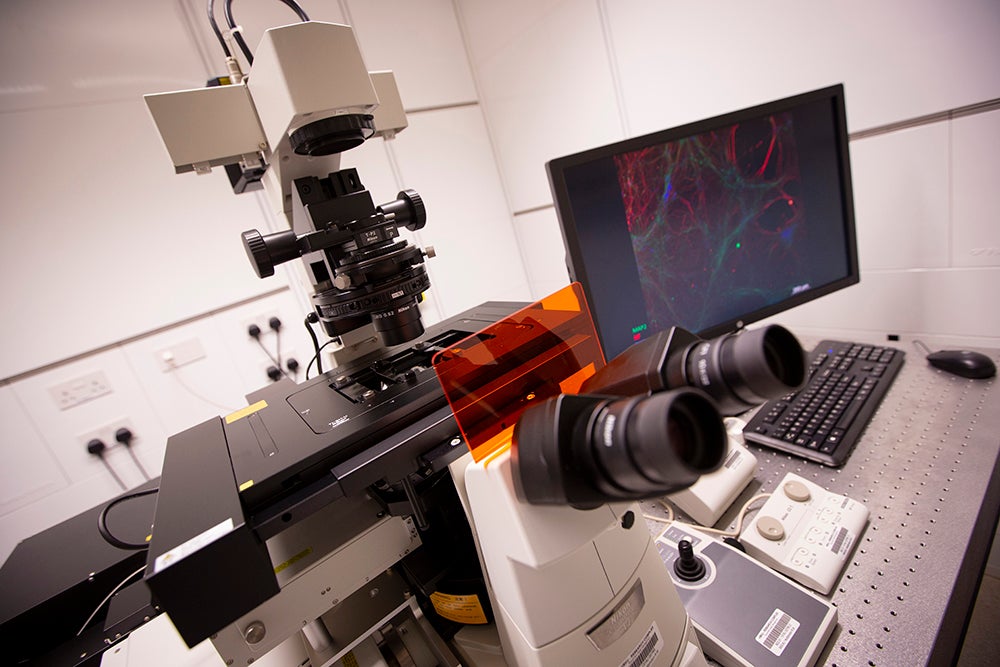
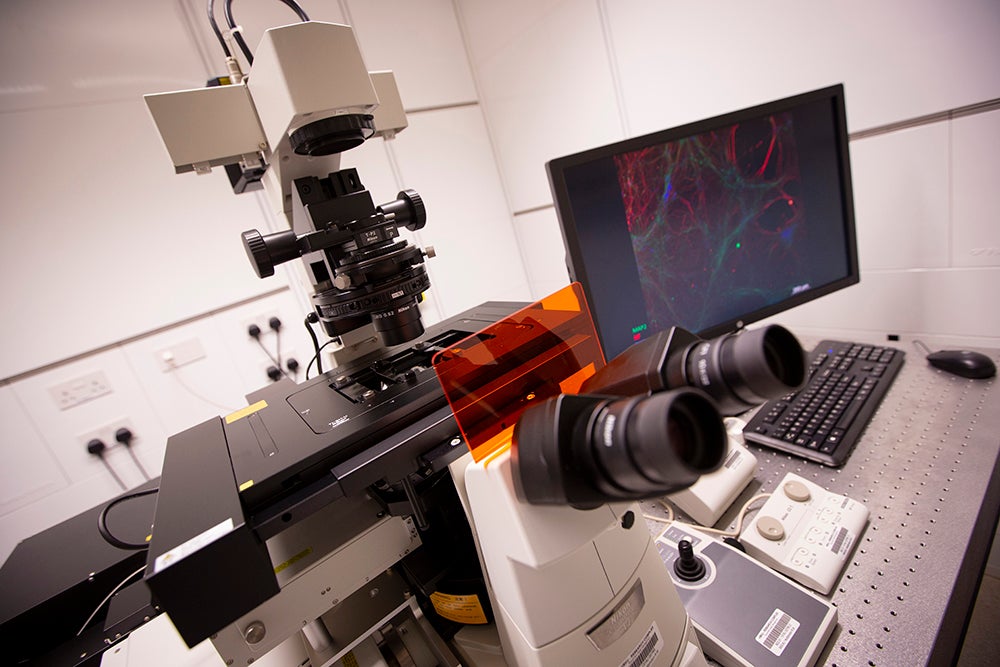
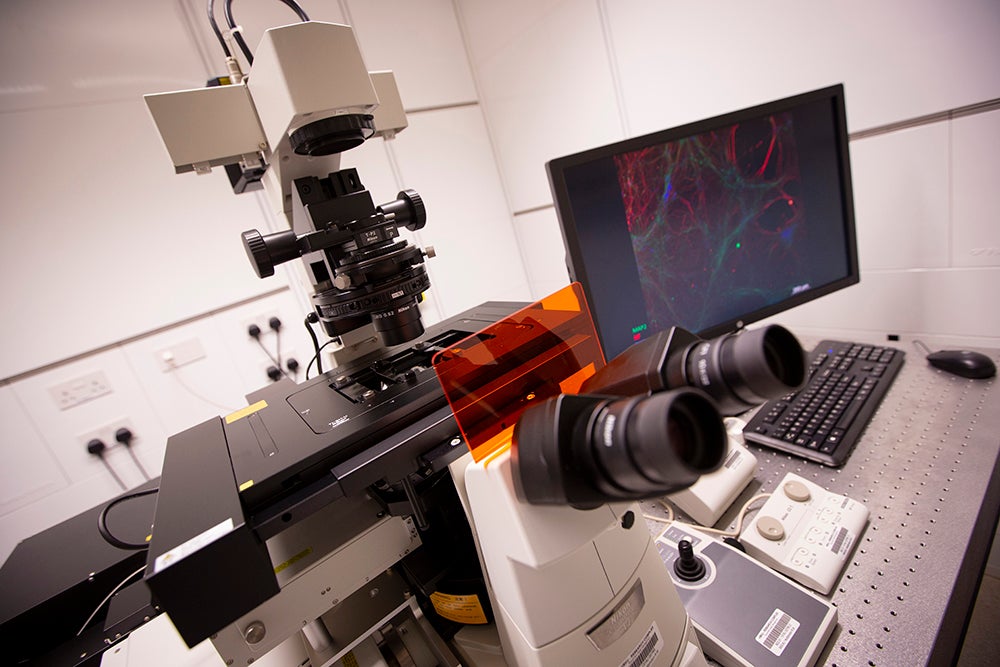
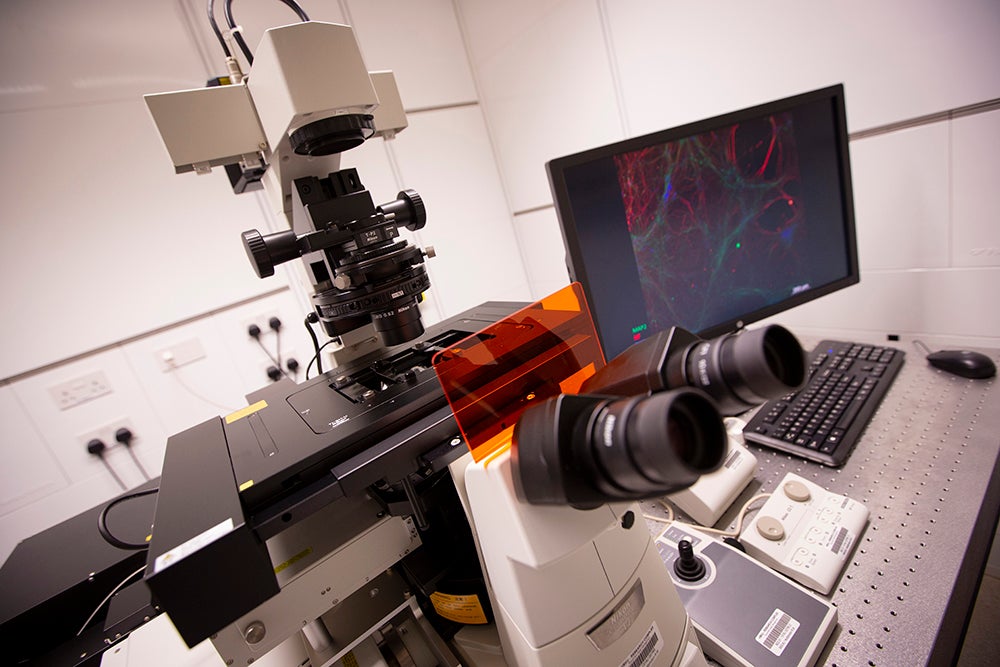
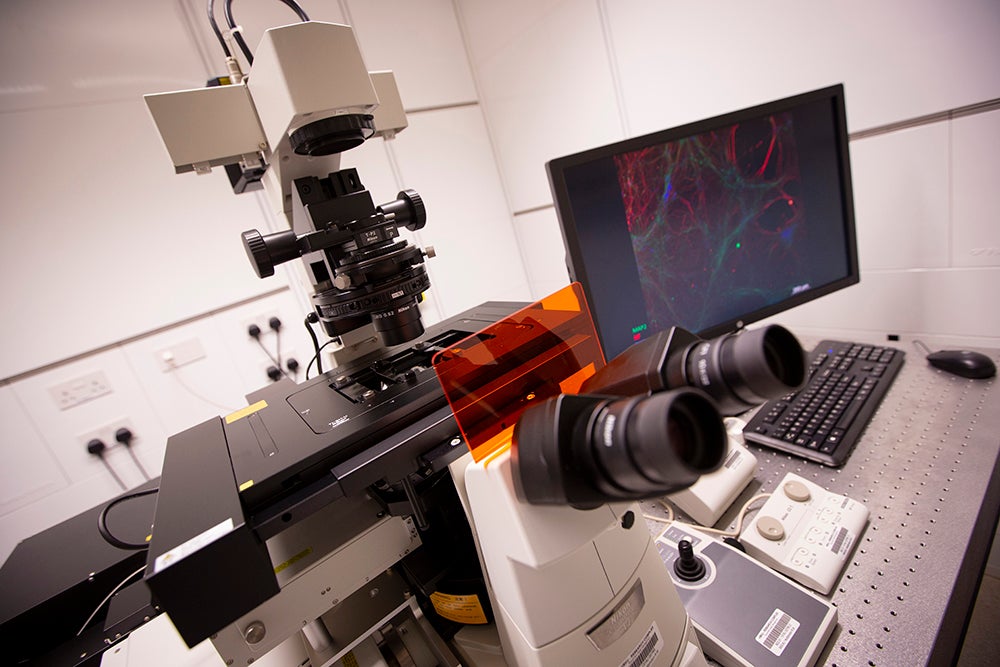
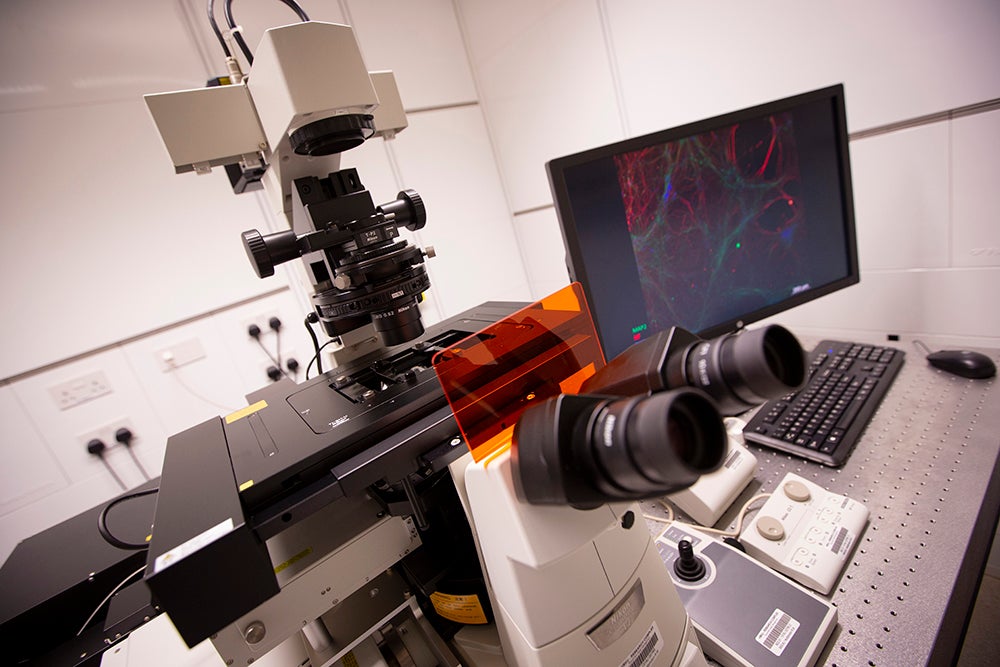
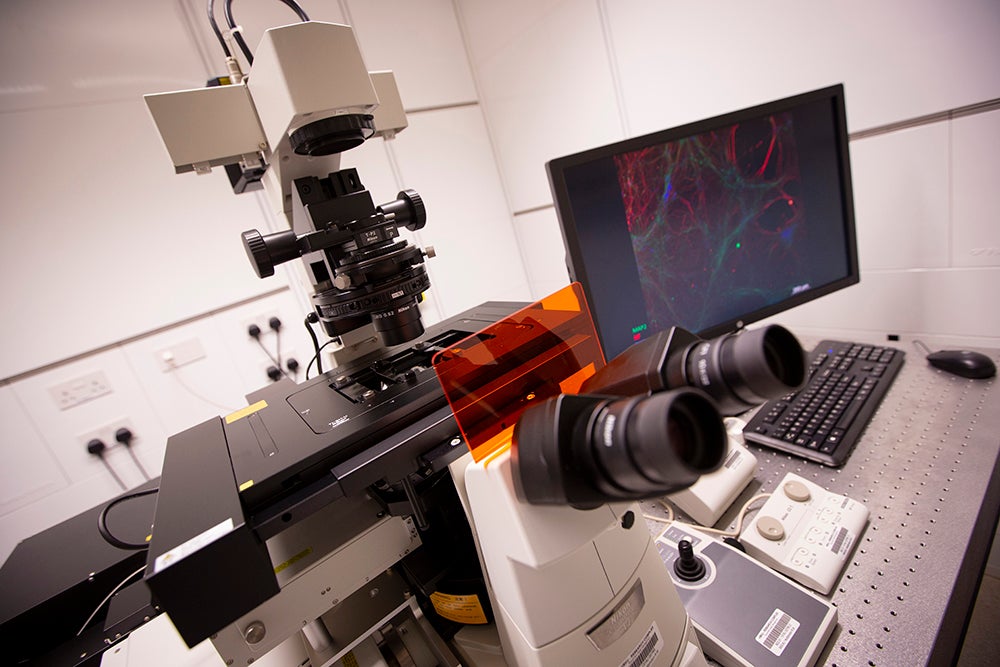
At Qatar Biomedical Research Institute (QBRI), which is a part of Qatar Foundation member Hamad Bin Khalifa University (HBKU), we are carrying out groundbreaking research in many areas, including Alzheimer’s disease.
QBRI has long been positioned as a pioneering national research institute that aims to improve healthcare through innovation in the prevention, diagnosis, and treatment of diseases, and we are proud of our Neurological Disorders Research Center, which focuses on neurodegenerative diseases.
The center enables various stakeholders to carry out extensive research on neurodegenerative diseases. The research conducted at the center is a precursor to identifying genetic and biological markers unique to the Arab population, to aid early diagnosis.
Of course, this is only part of what QBRI does, and we are also very proud of our Cancer Research Center and our Diabetes Research Center, among others.
As an innovation-centric university, HBKU leads the way in education and research that is dedicated to solving critical challenges facing Qatar and the world.
With around 50 million worldwide living with Alzheimer’s, it is essential that we continue to make major breakthroughs in this field.
Related News

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease
QBRI Joins Hands with Qatar University to Provide Research Analytical Services

QBRI Partners with PHCC and QCRI to Combat Prediabetes Through New Screening Tool

QBRI and Sultan Qaboos University Collaborate on Autism Spectrum Disorder Research

HBKU's QBRI Unveils Promising Arabic Stimuli: A Step Forward in Autism Spectrum Disorder (ASD) Diagnosis
Unveiling New Insights into Dementia: Autoantibodies and Blood-Based Biomarkers

Embracing the Colors of the Autism Spectrum: The Importance of Early Intervention and Advocacy

100-Year Anniversary of the Discovery of Insulin is of Great Relevance to QBRI

Qatar Biomedical Research Institute and Qatar University Scientists Conclude the International Symposium on Role of Glycation in Food-Health-Disease