Excellence QBRI Insights: Severe COVID-19 Immunopathology and Computed Tomography-Based Diagnosis
While the majority of COVID-19 patients experience mild symptoms, about 20% of cases develop severe pneumonia and respiratory failure. This week, QBRI experts discuss the hyper-activation of the immune defense system and detection of pneumonia by Computed Tomography (CT) in severe COVID-19 cases.
The immune landscape in severe COVID-19
The major elements of the human immune system (Figure 1) can be sub-classified as follows:
(1) commanders, for maturing and directing individually capable immune cells (helper T-cell/lymphocyte, ‘CD4+ T-cell’);
(2) fighters, fighting against enemy infections with cytotoxic molecules (cytotoxic T-cell, ‘CD8+ T-cell’) or with antibodies (B-cell/lymphocyte);
(3) calmers, to prevent the immune system going into overdrive (regulatory T-cell/‘Treg’);
(4) presenters, communicating information on the enemy invaders to T-cells (dendritic cells and macrophages); and
(5) other immune cells (e.g. neutrophils and natural killer cells).
Cytokine storms occurring in COVID-19 patients have been explained previously.
With a cytokine storm, a hyper-activated immune response ensues, resulting in severe tissue damage, pneumonia and increasing the risk of mortality (1, 2).
Several studies have shown decreased levels of total lymphocytes, CD4+ T-cells, CD8+ T-cells, B-cells, and natural killer cells in COVID-19 patients, with severe cases having even lower levels than mild cases (3-6). Moreover, patients with severe COVID-19 infection (identified by pneumonia) also experience elevated levels of neutrophils and cytokines such as interleukin (IL)-6, IL-10, IL-2 and interferon (IFN)-γ. A recent study, comparing features of CD4+ and CD8+ T-cells in peripheral blood between mild and severe COVID-19 groups in their first and third week of illness, showed an increased activation of CD4+ and CD8+ T-cells in the severe group compared with those in the mild group at the third week. Although cytokines such as IFN-γ, IL-2, and IL-4 were not different between the two groups, cytotoxic molecules, including perforin and granzyme B, were expressed at higher levels in both CD4+ and CD8+ T-cells in the severe group. In contrast, immune suppressive Tregs were decreased in the severe COVID-19 group compared to the mild group.
Taken together, these findings indicate that the immune system in COVID-19 patients with severe disease turns to more aggressive fighters with cytotoxic weapons and avoids calmers that could dampen the hyper-activated immune response (7). The number of individuals assessed in this study was quite small and requires replication in larger groups; however, similar observations have been made in other studies. A study investigating single cell RNA-sequencing data from bronchoalveolar lavage fluids of mild and severe COVID-19 patients reported hyper-activated CD4+ T-cells and reduced Tregs in the lung, resulting in lung damage (8). The hyper-activated state of the immune system has also been evidenced by markers of chronic activation and exhaustion on T-cells and natural killer cells (9-11).
It is not yet fully understood why COVID-19 infection precipitates such a dangerous immunological overdrive in some patients, although accompanying issues, such as advanced age and chronic conditions such as diabetes and cardiovascular disease, likely contribute to a debilitated and/or dysfunctional immune system.
Numerous clinical trials are currently assessing the efficacy of repurposing immunomodulatory drugs for treating COVID-19 (12). One such candidate is Toclizumab- an inhibitor of the IL-6 cytokine, which is generally used for the treatment of autoimmune diseases such as rheumatoid arthritis. Treatment with Toclizumab was shown to reduce the need for mechanical ventilation and death in severe COVID-19 cases in an Italian study, but its efficacy remains to be confirmed by ongoing trials (13). Despite this, the dilemma of ensuring a functional immune response while preventing hyper-activation still remains to be resolved to optimize management of severe COVID-19.
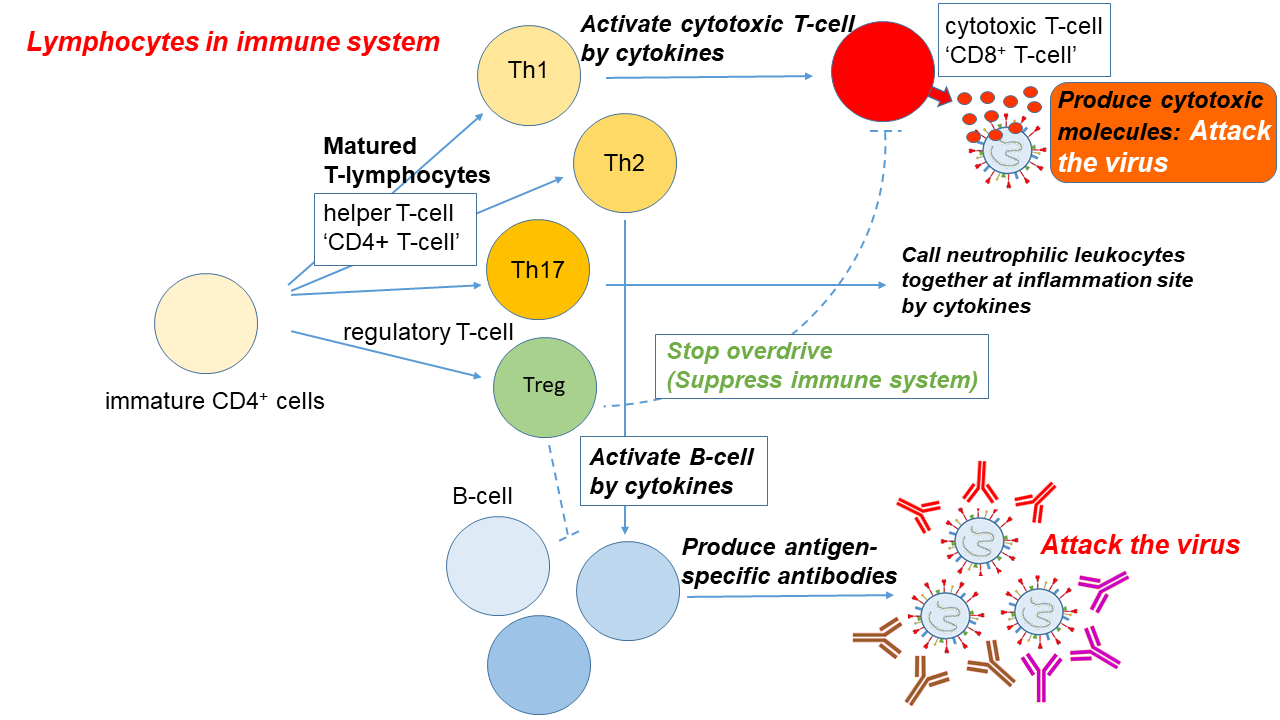
Figure 1. Immune response to a viral infection
Computed tomography (CT) scanning - a complementary COVID-19 diagnostic method
Although the COVID-19 reverse transcriptase polymerase chain reaction (RT-PCR) test is still the gold-standard diagnostic method, several reports have highlighted the role of computed tomography (CT) as a valuable tool for COVID-19 diagnosis (14-16). CT is one of the most prevalent medical imaging methods, which uses a series of x-ray images to generate a cross-sectional image of organs (Figure 2). In addition to its performance and simplicity, CT can quickly detect lung abnormalities and enable imaging diagnoses at an early disease stage (16).
A study on 81 patients in Wuhan, China, indicated that COVID-19-associated pneumonia, a characteristic of severe disease, manifests with an abnormal CT, even at an early asymptomatic stage (17). At early stages of infection, patients showed predominantly unilateral, though multifocal, areas of the distinctive ground-glass opacity on lung CT and, as the disease progresses, the opacity becomes more diffuse and is observed in both lungs. In fact, the value of the CT has been proven in many patients showing false negative RT-PCR results. CT examination performed in a Chinese patient cohort, where there was suspicion of COVID-19 but the initial RT-PCR test was negative, revealed that a significant proportion of CT positive cases did have the disease based on positive results from a subsequent RT-PCR test (14). Furthermore, about 40% of the cases showed improvement in follow-up CT scans prior to testing negative by RT-PCR, indicating that CT scans may additionally be an early indicator of disease resolution.
Another recent study reported that about 90% of suspected COVID-19 patients showed a high detection rate of viral pneumonia when these patients underwent chest CT (16). An additional Chinese study in 36 patients diagnosed with COVID-19 pneumonia revealed that the sensitivity of CT examinations was 97.2%, whereas RT-PCR sensitivity was 84.6% (18).
Based on CT images, recent work has proposed an artificial intelligence (AI) model to differentiate COVID-19 from pneumonia caused by other types of viruses (19, 20). The computational model revealed a 90% sensitivity and 95% specificity in detecting COVID-19. Thus, combining CT imaging with clinical and laboratory assessment could allow the early diagnosis and intervention for severe COVID-19.
As per the current World Health Organization (WHO) recommendations, chest CT is recommended in cases when RT-PCR testing is not available; where RT-PCR testing is available, but results are delayed; and where initial RT-PCR testing is negative, but there is a high clinical suspicion of COVID-19 infection. While the widespread availability and rapidity of CT scans are advantageous during the pandemic, its limitations include non-specificity, requiring confirmation with alternative diagnostic tests, and radiation exposure, which may not allow its utility for screening pregnant women and young children.
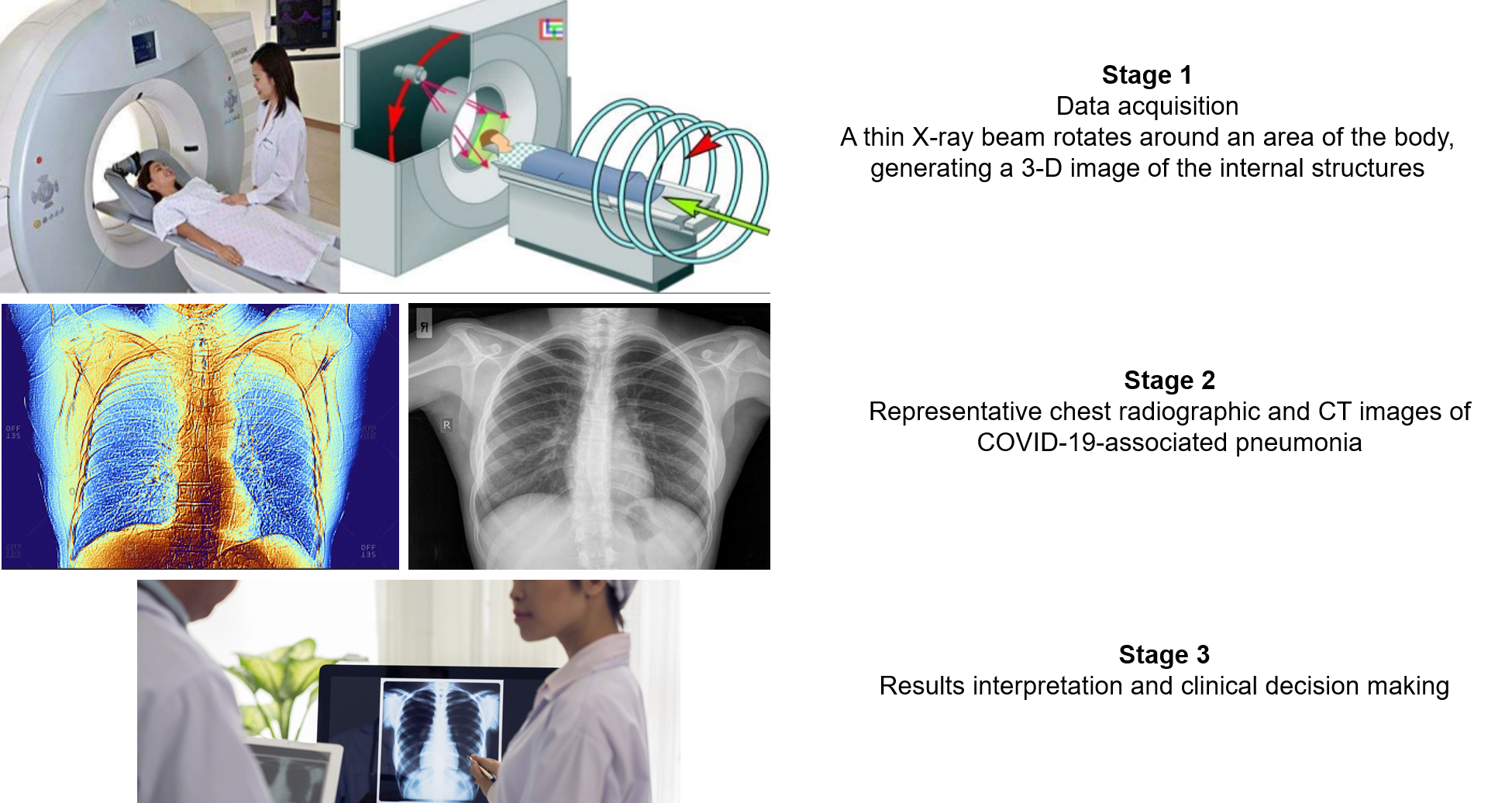
Figure 2. Computed Tomography (CT)-based diagnosis for COVID-19
Images accessed from: Link
Section Contributors:
The immune landscape in severe COVID-19: Dr. Yoshie Kobayashi (Postdoctoral Researcher, QBRI)
Computed tomography (CT) scanning- a complementary COVID-19 diagnostic method: Dr. Afif Ben Mahmoud (Senior Research Associate, QBRI)
Illustration by: Dr. Yoshie Kobayashi
Arabic text validation: Dr. Nour K. Majbour (Research Associate, QBRI)
Editors: Dr. Adviti Naik (Postdoctoral Researcher, QBRI) and Dr. Alexandra E. Butler (Principal Investigator, QBRI)
For references, please click here.




