By Dr. Mariam Al-Muftah and Reem Elasad

October marks the month of Breast Cancer Awareness worldwide with the aim of increasing awareness and highlighting the importance of regular screening and early detection. Hamad Bin Khalifa University’s (HBKU) Qatar Biomedical Research Institute (QBRI) has published several detailed Insights over the past few years, highlighting the necessity of early screening and detection, precision medicine’s contribution to treatment, and research efforts in the field. The latest considers efforts to develop vaccines as a potential treatment option for breast cancer patients.
Breast cancer is the most common cancer diagnosed among women worldwide, accounting for approximately 1 in 4 cancer cases and 1 in 6 cancer deaths. According to QBRI’s analysis of 2018 cancer statistics, Arab-speaking countries show higher breast cancer incidence and mortality rates compared to the rest of the world. The World Health Organization also projects rising cancer incidence in the coming years due to population growth, aging, and increased exposure to risk factors.
As the incidence and burden of breast cancer increases, early detection and treatment are the most effective means for improving patient outcomes. Patients diagnosed at early stages of breast cancer (i.e. stage I, where cancer has not spread to nearby lymph nodes) show a survival rate of more than 98% during the first 5 years post-treatment. Despite efforts to increase awareness and encourage regular early cancer screening programs, not all patients are diagnosed at early stages. With higher incidence and mortality rates in Arab-speaking countries, there is a pressing need to build on existing efforts and intensify outreach to ensure all women undergo regular screening and early detection, with the hope of saving more lives.
Current Treatment Options
Breast cancer is divided into different subtypes based on the expression of markers such as Estrogen receptors (ER) and Human-epidermal growth factor receptor 2 (HER2). Breast cancers that lack either the expression of ER and HER2 are known as triple-negative breast cancer (TNBC) and is considered the most aggressive subtype. Treatment options differ based on the cancer subtype and stage at diagnosis. The standard of care includes surgery, radiotherapy, targeted therapy, and chemotherapy.
In recent years, immunotherapy has revolutionized cancer treatment and has been approved (in combination with chemotherapy) for breast cancer, including TNBC. Cancer develops due to its ability to escape detection by the immune system, therefore the rationale behind immunotherapy is to provoke the immune system to recognize, target and eliminate cancer cells with minimal effect on normal cells. Several immunotherapy approaches exist, including targeting a group of proteins known as immune checkpoints, which normally control the immune system’s response to the body’s own cells. Targeting immune checkpoints with inhibitors in combination with chemotherapy has recently been approved by the Food and Drug Administration (FDA) for the treatment of TNBC and HER-positive patients. Despite its limited eligibility, this approach has shown promising outcomes and offers hope to patients who do not have other treatment options.
Vaccine Developments
Another form of immunotherapy involves cancer vaccines. Cancer cells can be identified by either expressing a unique marker, markers that have risen due to mutations (neoantigen), or normal proteins that are produced at much higher levels by cancer cells compared to healthy cells. The concept of a cancer vaccine seeks to take advantage of these differences to stimulate and direct the immune system against specific markers present in cancer cells and eliminate them. Theoretically, targeting unique cancer markers such as neoantigens allows for the precise elimination of cancer cells with minimal to no effect on healthy cells.
Vaccines are classified according to composition, such as nucleic acid (RNA or DNA), carbohydrate, whole-cell or peptide (a small part of a protein). Major advancements have been made in the field of vaccine technology, over the past two decades. Despite differences in composition, delivery, and design, all vaccines function by providing instructions to the immune system to trigger a response against a specific target.
In recent years, breast cancer vaccines have made notable progress beyond the development phase and are being tested in clinical trials in patients. One of the most studied vaccines is NeuVax™ against E75, a peptide that provokes an immune response against the HER2 protein in patients with tumors that show high levels of HER2 (a subset of breast cancer). In phase I and II clinical trials, the vaccine showed promising tolerance and response in patients, despite limited responses observed during phase III. Studies are currently underway to assess whether NeuVax™ can offer a lifespan advantage and lower recurrence in patients.
Similarly, there are ongoing clinical trials testing vaccines for TNBC, with the hope of developing effective therapies to treat this aggressive subtype. A particularly promising example involves a vaccine against alpha-lactalbumin, a protein expressed at high levels in 70% of TNBC patients. Alpha-lactalbumin is a ‘retired protein’, meaning it is normally only found during certain stages and tissues (in this case, in the breast during late-pregnancy and lactation) and is no longer expressed by healthy cells. Provoking an immune response against this protein could uniquely target cancer cells while sparing healthy ones. Recent press releases report that several early-phase clinical trials are ongoing at the Cleveland Clinic, involving two groups: patients who have had TNBC and are at risk of recurrence; and cancer-free individuals who have a genetic risk developing TNBC. Vaccination of the second group will determine whether the vaccine can also prevent TNBC development.
In parallel, advances have been made in technologies such as mRNA vaccines. These vaccines provide instructions to cells to produce a protein or peptide to generate an active immune response against it. This technology offers several advantages, including rapid production of large quantities, and the ability to carry information for multiple targets. There are two methods to deliver mRNA vaccines to breast cancer patients: either loading mRNA into a type of immune cell called Dendritic cells and reinfusing them into the patient or using nanoparticle-based mRNA vaccines, which are directly injected into patients. Several breast cancer-specific mRNA vaccines have been developed and have either completed early phase clinical trials or are recruiting patients. These include the VPR-HER2 vaccine, which targets HER2 and has shown tolerability and promising initial outcomes in breast cancer patients.
Future Prospects
Despite advances in treatment, breast cancer recurrence remains a challenge. It is believed that cancer vaccines may be an effective means of treatment and preventing recurrence, as they theoretically provide a long-lasting immune response against a particular marker present in cancer cells.
While many breast cancer vaccines utilizing different technologies have been developed and shown promising outcomes in early-phase clinical trials, large-phase II or III clinical trials have not yet shown significant therapeutic advantages. This could imply that these vaccines have insufficient long-lasting impact. While this field faces challenges, the concept of directing the immune system against cancer cells nevertheless remains promising. Further testing, along with continued development and optimization of vaccines, will lead to more effective and individualized treatment options for breast cancer patients. Several clinical trials are currently running to test the efficiency of vaccines in eliminating breast cancer cells, preventing recurrence, or the onset of cancer in high-risk individuals. These will provide further information and a deeper understanding of the potential of vaccines for treating breast cancer.
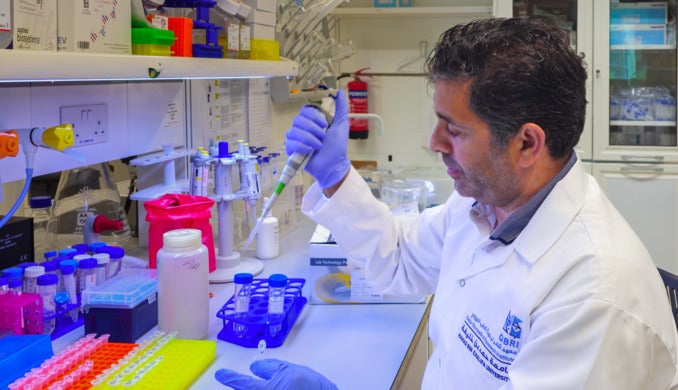
Dr Mariam Al-Muftah is a scientist in the Translational Oncology Research Center at Hamad Bin Khalifa University’s (HBKU) Qatar Biomedical Research Institute (QBRI).
Reem Elasad is research assistant in the Translational Oncology Research Center at Hamad Bin Khalifa University’s (HBKU) Qatar Biomedical Research Institute (QBRI).
Arabic text validation: Rowaida Z. Taha, Senior Research Associate, QBRI.
The thoughts and views expressed are the author’s own and do not necessarily reflect an official University stance.