FDA-Approved Alzheimer’s Drug Will Help Spur Innovation Toward Personalized Therapies

September marks Alzheimer’s Awareness Month and Dr. Omar El-Agnaf, Executive Director of Qatar Biomedical Research Institute at Hamad Bin Khalifa University, explains why the first approved treatment for the disease for nearly 20 years must go hand in hand with biomarker-supported diagnosis and personalized therapies.
Alzheimer’s is a neurodegenerative disease that is clinically diagnosed as a form of dementia. Mostly identified in those aged 65 and above, Alzheimer’s is the onset of a progressively degenerative form of memory loss and it impacts patients and their families physically, psychologically, socially, and economically.
Treatment for Alzheimer’s is normally administered in the form of certain prescription drugs. This treatment could briefly mitigate memory loss, but the medications generally come with many side effects. Doctors recommend such medications for temporary use as the side effects outweighed any positive short-term impact.
However, this year saw a breakthrough when the US Food and Drug Administration (FDA) granted accelerated approval for the first novel drug to treat Alzheimer’s disease in nearly 20 years, bringing welcome news for those living with the disease and their families. Similar to any other approved drug, the FDA has concluded that the benefits outweigh the potential risks. Aducanumab, manufactured by Biogen Inc. and pharmaceutical company Eisai, is the first therapy to attack the underlying disease process and slow down its impact.
The approval of the drug comes at a time when there is an extremely high death rate among people with dementia globally due to the pandemic, according to Alzheimer’s Disease International.
 When approving the drug, the FDA said there is ‘substantial’ evidence that aducanumab (branded Aduhelm) reduces amyloid-beta plaques. In the brain of an Alzheimer’s patient, abnormal clusters of a protein called beta-amyloid build up in and around nerve cells, disrupting their function, and eventually leading to brain-cell death. By clearing amyloid in the brain, aducanumab slows disease progression, making it meaningful for many patients with early symptomatic Alzheimer’s disease.
When approving the drug, the FDA said there is ‘substantial’ evidence that aducanumab (branded Aduhelm) reduces amyloid-beta plaques. In the brain of an Alzheimer’s patient, abnormal clusters of a protein called beta-amyloid build up in and around nerve cells, disrupting their function, and eventually leading to brain-cell death. By clearing amyloid in the brain, aducanumab slows disease progression, making it meaningful for many patients with early symptomatic Alzheimer’s disease.
Aducanumab is not yet available worldwide so in some countries the traditional treatment will still be used, but this is indeed an important breakthrough and I am greatly encouraged that we now have an FDA-approved drug that can be effective in the early stages of Alzheimer’s. This devastating, degenerative brain disease, the most common type of dementia, is a major problem worldwide.
There has been controversy over the FDA’s decision, even from the general public’s side, but it is supported by scientific evidence from two large-scale phase 3 clinical trials involving thousands of patients. Although the FDA approved the drug, reflecting their trust in the safety and reliability of the drug, they will continue to closely monitor its use. The accelerated approval pathway now requires Biogen to conduct another randomized, controlled trial to confirm that the drug, taken as a monthly intravenous infusion, is clinically effective in slowing cognitive decline.
As a scientist and a researcher, I believe that a research breakthrough relating to the very early stage of Alzheimer’s gives us a better chance of tackling the disease. It is also my view that it is now essential that we continue conducting research to find drugs for all stages and all types of dementia.
Alzheimer’s is a heterogeneous (diverse in character or content) disease, especially at an advanced stage. It rarely has one cause and its symptoms may overlap with other dementia-related diseases. Misdiagnosis can lead to delayed treatments or even receiving incorrect treatment. These risks underscore the need for very good diagnostic markers to identify those who are at the early stage of Alzheimer’s before they even show any clinical symptoms.
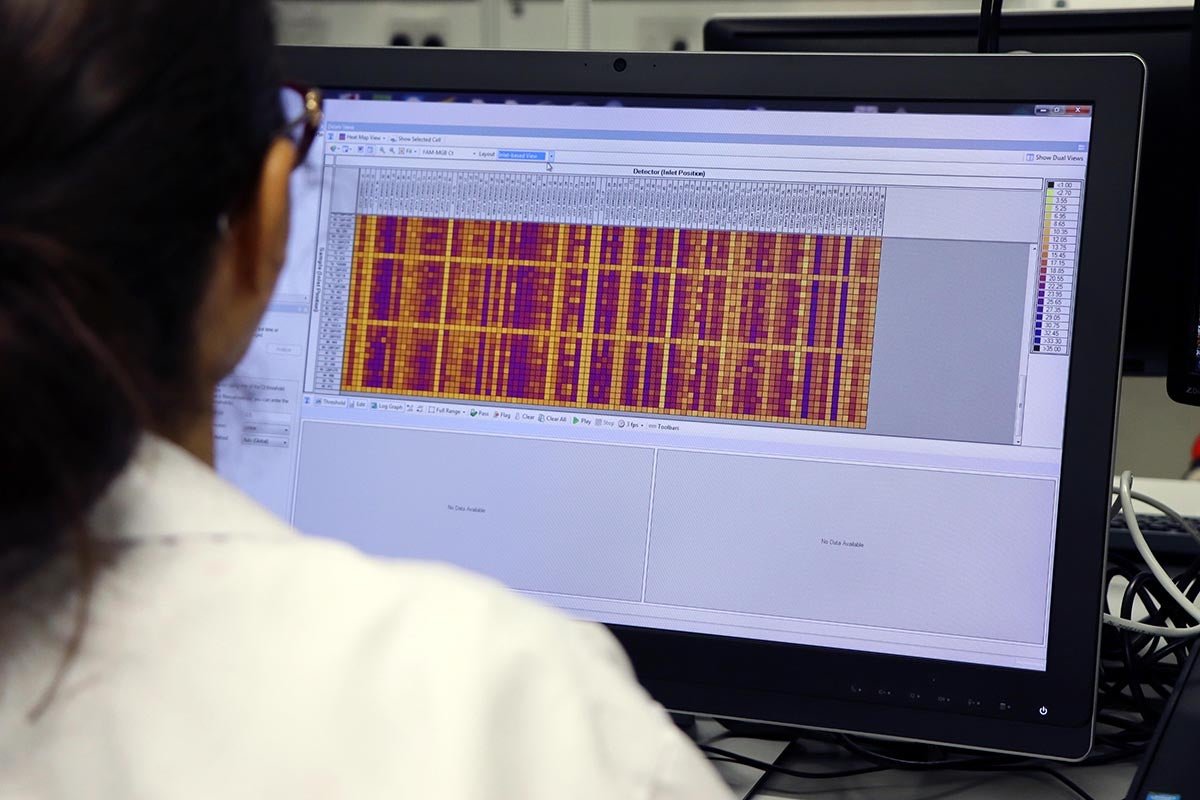
Indeed, there has been great progress in the last 15-18 months in developing a blood test biomarker to identify Alzheimer’s disease patients in the early stages. The test measures biomarkers that frequently reflect the presence of amyloid plaques in the brain as well as the presence of a gene variant that increases the risk of the disease.
Prescreening patients with a blood test rather than brain imaging or cerebrospinal fluid could ultimately lower the exorbitant cost of clinical drug trials. Other advantages are being able to accurately screen patients that may qualify for experimental drugs.
The developments are very significant for the scientific research community as we press on with research efforts toward finding a treatment for the advanced stages of Alzheimer’s disease and other types of common dementia such as dementia with Lewy bodies, Parkinson’s disease with dementia, etc.
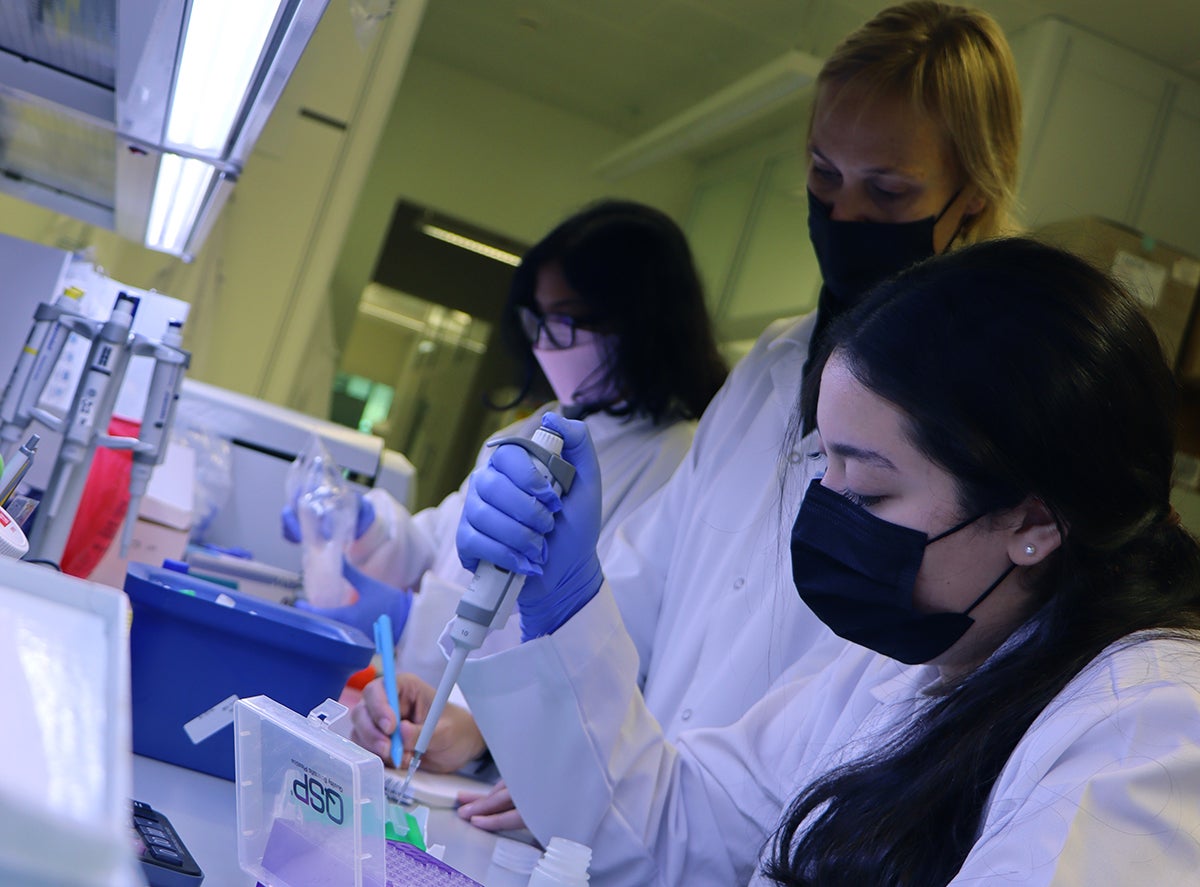
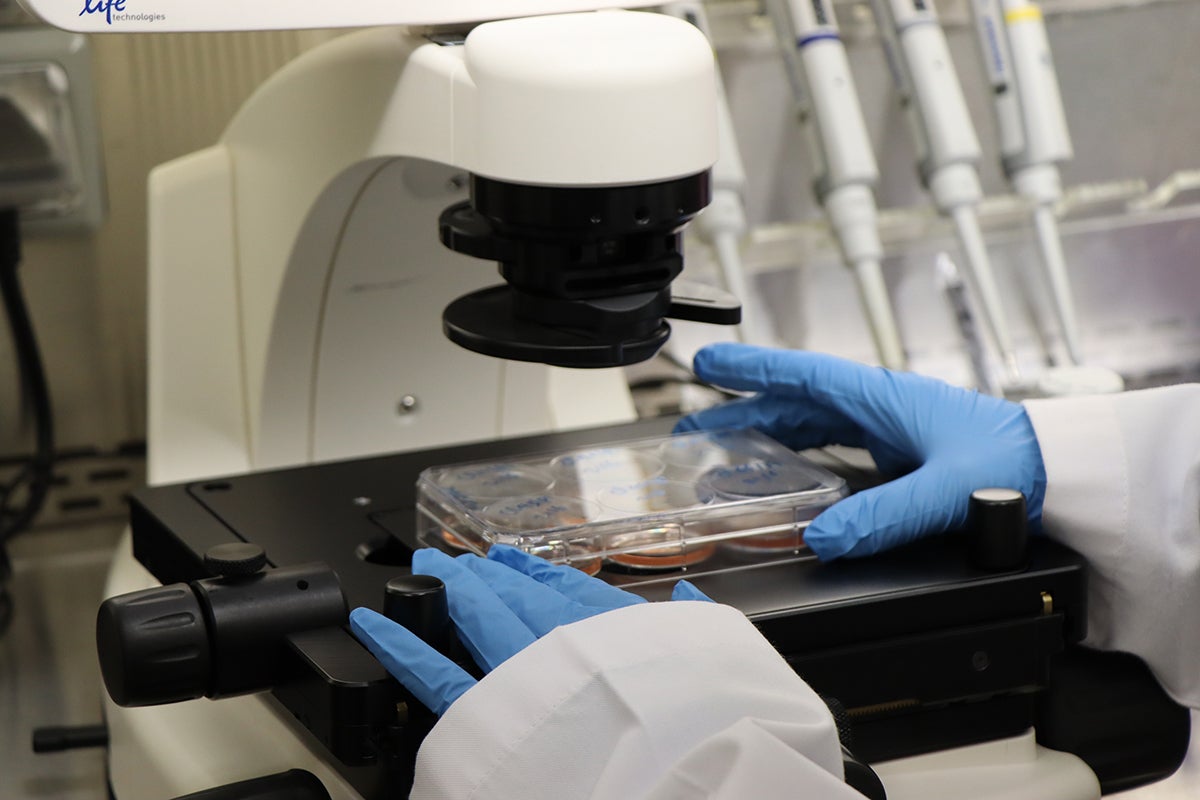
At Qatar Biomedical Research Institute (QBRI), part of Qatar Foundation and Hamad Bin Khalifa University, our pioneering Neurological Disorders Research Center (NDRC) is investigating the genetic and genomic background underpinning a number of neurological disorders including Alzheimer’s disease.
Our research at NDRC has the potential to greatly impact the visibility of neurological disorders in Qatar and the region, by researching new treatments and significantly accelerating the pace of therapeutic development using technologies such as experimental disease modeling, stem cell biology, and novel biomarker analyses.
Novel biomarkers are essential for identifying what kind of pathology develops in patients and for developing individually-tailored effective therapies. In terms of biomarker discovery, the field is moving forward in a promising way, and the NDRC team is making huge progress in this important area.
The FDA approval of aducanumab is sure to encourage other pharmaceutical companies and funding agencies to sustain and even increase investments in drug discovery for neurodegenerative diseases. Hopefully this will lead to other breakthroughs to develop a more personalized treatment for Alzheimer’s and other neurodegenerative diseases.
Dr. Omar El-Agnaf is the executive director of Qatar Biomedical Research Institute, part of Hamad Bin Khalifa University.
This article is submitted on behalf of the author by the HBKU Communications Directorate. The views expressed are the author’s own and do not necessarily reflect the University’s official stance.
Related News

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention

Huge Potential of HBKU’s Qatar Biomedical Research Institute Convinced Dr. Nasser Hussein Zawia to Accept Opportunity as Research Director

QBRI Insights: Medical Problems and Comorbid Conditions Associated with Autism

Can Gene Signatures Explain Why Some Breast Cancers Are Resistant to Chemotherapy?

QBRI Insights: Extracellular Vesicles as Novel Biomarkers and Therapeutic Targets for Neurological Disorders

Alzheimer’s Disease – Warning Signs, Available Treatments and the Guidelines for Prevention