Once regarded as the preserve of parts of the world where sedentary lifestyles had usurped physical activity, Diabetes Mellitus (DM) has now evolved into a truly global health challenge. According to a 2021 report by the International Diabetes Federation (IDF) an estimated 537 million adults worldwide are living with diabetes, a figure that is projected to increase to 783 million by 2045 if no proactive measures are taken. With almost 20% of its population considered diabetic, Qatar ranks among the top 10 countries in the world with the highest prevalence of Diabetes Mellitus.
Poorly managed diabetes can result in a number of micro- and macrovascular complications, such as heart failure, blindness, nephropathy, neuropathy, foot ulceration/amputation, and death. While the exact etiology of DM remains incompletely understood, mounting evidence suggests a complex interplay between environmental and genetic factors. With this in mind, the exponential rise in incidences of Type 2 Diabetes (T2DM) over the past few decades prompts an exploration of the environmental factors driving this surge. While genetics play a crucial role in susceptibility, the observation of an escalating prevalence in genetically stable populations points towards the paramount influence of contemporary lifestyles. Sedentary habits, coupled with the consumption of high calorie-abundant foods, have become hallmark characteristics of modern living. These lifestyle choices contribute significantly to the development and progression of T2DM.
Obesity Triad Dynamics
A central theme in the environmental contribution to T2DM is the increased availability and access to calorie-dense food and reduced physical activity. Modern societies have witnessed a shift towards processed foods that are high in refined sugars and unhealthy fats. This dietary transition, combined with a decline in physical activity levels, has created an obesogenic environment. Obesity, a well-established risk factor for T2DM, is strongly associated with insulin resistance and impaired glucose metabolism. Put simply, being overweight or obese significantly increases the risk of developing T2DM.
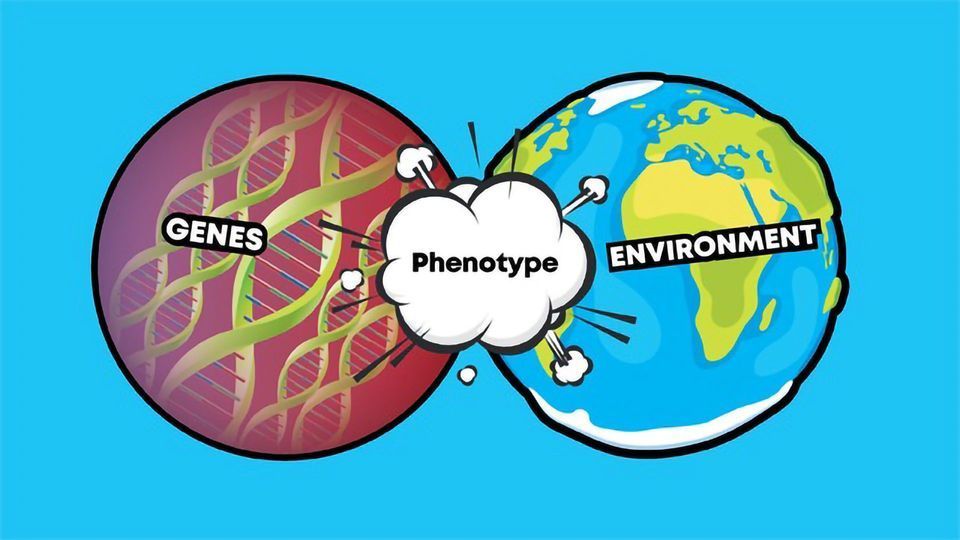
While environmental factors are pivotal, the genetic component of T2DM cannot be overlooked. Familial clustering and heritability studies indicate a genetic predisposition, with certain populations exhibiting a higher prevalence of the disease. Specific genetic variants, particularly those influencing insulin metabolism, have been identified as contributing factors. Genome-wide association studies (GWAS) have uncovered multiple susceptibility loci associated with T2DM, shedding light on the genetic underpinnings of the disease.
The interplay between genetics and the environment is complex, with gene-environment interactions playing a crucial role in T2DM development. Individuals with a genetic predisposition may remain asymptomatic if not exposed to specific environmental triggers. Conversely, individuals without a strong genetic predisposition can develop T2DM if exposed to unfavorable environmental conditions. This dynamic interaction underscores the importance of understanding both genetic and environmental factors for better treatment and management of the disease.
Promising Treatment Options
Recognition of the intricate interplay between genetics and the environment in T2DM has significant implications for preventive strategies and treatment approaches. Lifestyle modifications, including caloric restriction and increased physical activity, emerge as first-line interventions in clinical settings. These measures aim to address the environmental contributors to T2DM, emphasizing the importance of adopting healthier habits to mitigate the risk and manage the disease.
As the understanding of environmental influences deepens, precision interventions can be tailored to address the root causes of T2DM. Focusing on lifestyle modifications aligns with the idea that altering environmental conditions can significantly impact disease outcomes. Harnessing this knowledge allows for more effective and targeted interventions specially for those with genetic predisposition, providing a promising avenue for personalized medicine to optimize treatment outcomes in the battle against T2DM.
The recent entry of so-called “wonder” drugs from several pharmaceutical companies also offers hope for the diabetic population. In the past, metformin and other small molecule compounds have played a large role in minimizing symptoms of the disease. However, many of the new peptide-based drugs, which mimic a hormone that helps to control blood sugar levels, might also be useful for protecting individuals from heart and kidney disease.
The surge in T2DM finds its roots predominantly in environmental factors, with contemporary lifestyles playing a central role in disease incidence. While genetics contribute to susceptibility, it is the overwhelming impact of modern living that has fueled the diabetes epidemic. Addressing these environmental contributors through targeted lifestyle modifications stands as the linchpin in preventing and managing T2DM, offering a pathway to curb the rising tide of this chronic metabolic disorder. New medications also offer hope for improving the quality of life of affected individuals.
Section Contributors
Contributed by: Dr. Abdoulaye Diane (Postdoc, QBRI), Dr. Razik Abdulmuumin (Research Associate, QBRI), & Asma Allouch (Research Assistant, QBRI)
Arabic text validation: Rowaida Taha (Research Associate, QBRI)
Editor: Dr. Prasanna Kolatkar (Senior Scientist, QBRI)